Speaker
 Ehab Akkary, MD, FACS, FAACS
Ehab Akkary, MD, FACS, FAACS
Akkary Surgery Center, Morgantown, WV
Dr. Akkary started his practice in 2008 as an Academic Bariatric Surgeon and gradually shifted to Community based Cosmetic Surgery. He is Board Certified in General Surgery by the ABS and Board Certified in Cosmetic Surgery and Facial Cosmetic Surgery by the American Board of Cosmetic Surgery and the American Board of Facial Cosmetic Surgery. He practices in WV and PA where he performs wide variety of Cosmetic Surgery at AAAHC accredited facilities. Dr. Akkary is devoted to the field of Cosmetic Surgery, he is a Fellow of the AACS. He serves multiple committees at the AACS and the ABCS and he is a reviewer for multiple journals including JAACS.
Abstract
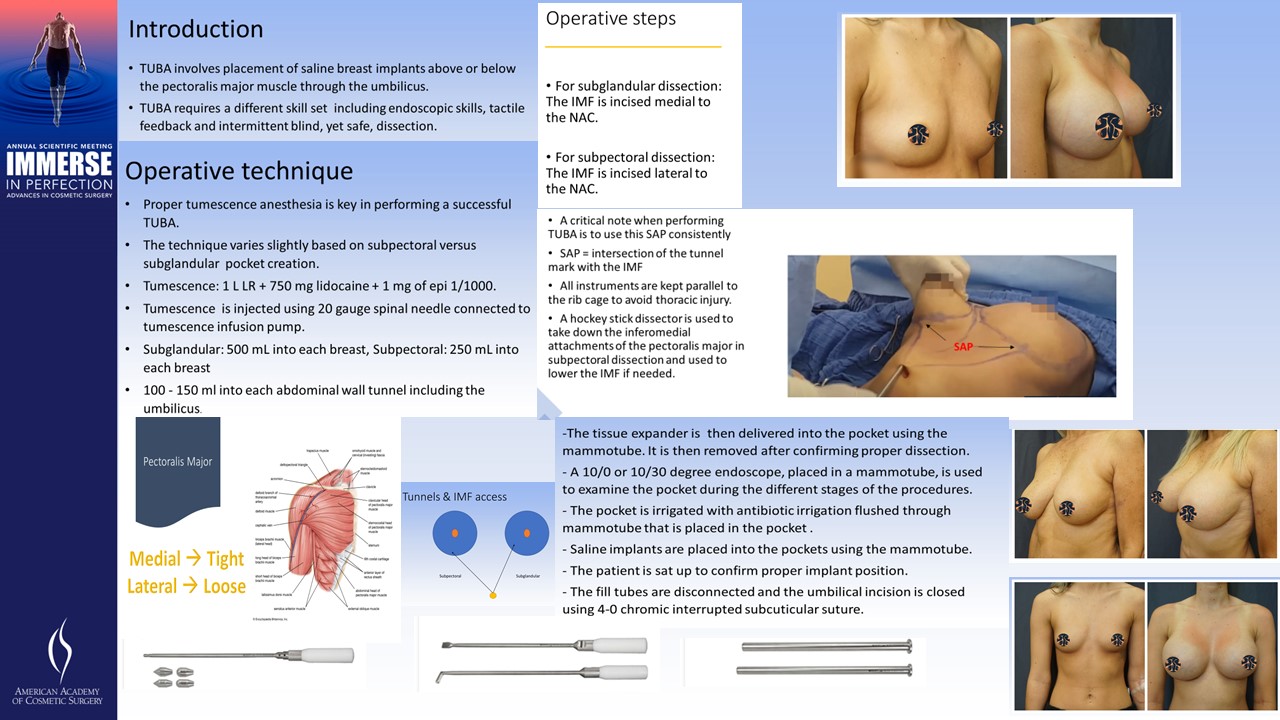
Introduction: TUBA involves placement of saline breast implants above or below the pectoralis major muscle through the umbilicus. TUBA, while implementing the principles of breast augmentation utilized in other approaches as periareolar, trans axillary or inframammary, it requires a different skill set including endoscopic skills, tactile feedback and intermittent blind, yet safe, dissection. Here, I present our technique for TUBA. the technique varies with subpectoral versus subglandular placement of the implants.
Operative technique: Proper tumescence anesthesia is key in performing a successful TUBA. The technique very is slightly based on subpectoral versus subglandular pocket creation. In our practice, tumescence is prepared using 1 L of lactated Ringer's mixed with 750 mg lidocaine and 1.5 mg of epinephrine 1/1000. Tumescence is injected using 20 gauge spinal needle connected to tumescence infusion pump. usually 500 mL of tumescence is injected into each breast in subglandular TUBA, 250 mL in subpectoral and 100 - 150 ml into each abdominal wall tunnel including the umbilicus.
Tumescence technique for subglandular TUBA:
- The breast is gently lifted and the subglandular plane is accessed medial to the nipple areolar complex (NAC).
- The needle is kept in parallel position to the rib cage to avoid violation of the pleural space.
- After infusing enough volume medially, The lateral subglandular plane is injected.
- Tumescence is infiltrated into the umbilical region and the planned subcutaneous abdominal wall tunnels.
Tumescence technique for subpectoral TUBA:
- The lateral edge of the pectoralis major muscle is lifted up laterally and the initial access is under the lateral edge of the muscle.
- The needle is kept in parallel position to the rib cage to avoid violation of the pleural space.
- The breast is firmly lifted and the subpectoral plane is accessed lateral to the nipple areolar complex (NAC).
- The medial part of the pocket is infiltrated by placing the needle under the muscle parallel to the ribs.
Operative steps:
- The incision is created using 15 blade scalpel under the under the superior umbilical fold respecting the boundaries of the umbilical ring.
- Long scissors are used to dissect the subcutaneous tunnels.
- Bullet dissectors are then used, in gradually increasing size, to access the planned pocket through the inframammary fold (IMF).
- For subglandular dissection: The IMF is incised medial to the NAC.
- For subpectoral dissection: The IMF is incised lateral to the NAC.
- A critical note when performing TUBA is to use this SAP consistently as the only access to the pocket during the entire procedure. The error of creating multiple access points will weaken the inframammary attachments and can eventually lead to bottoming out of the implants.
- All instruments were kept parallel to the rib cage to avoid thoracic injury.
- A hockey stick dissector is used to take down the inferomedial attachments of the pectoralis major in subpectoral dissection and used to lower the IMF if needed.
- The tissue expander is then delivered into the pocket using the mammotube. It is then removed after confirming proper dissection.
- A 10/0 or 10/30 degree endoscope, placed in a mammotube, is used to examine the pocket during the different stages of the procedures.
- The pocket is irrigated with antibiotic irrigation flushed through mammotube that is placed in the pocket .
- Saline implants are placed into the pockets using the mammotube.
- The patient is sat up to confirm proper implant position.
- The fill tubes are disconnected and the umbilical incision is closed using 4-0 chromic interrupted subcuticular suture.
Take Home Message
TUBA is an underutilized approach for breast augmentation. The procedure is virtually scarless and while it needs different skill set than traditional approaches for breast augmentation, Surgeons can adopt it to their practice and reach the learning curve by following a systematic standardized approach for the surgery.
