Speaker
 Donovan S. Reed, MD
Donovan S. Reed, MD
Texas Oculoplastics Consultants - TOC Eye and Face, Austin, TX
Doctor Donovan Reed graduated Summa Cum Laude with Honors from East Tennessee State University with a degree in Chemistry. He then commissioned as an officer in the United States Air Force and graduated as class Valedictorian from the Uniformed Services University where he was elected to Alpha Omega Alpha. Doctor Reed completed his Internship in General Surgery and his Ophthalmology Residency at the San Antonio Uniformed Services Health Education Consortium where he served as Chief Resident of the Ophthalmology Residency. During his residency training, he was awarded the USAF Commendation Medal for meritorious service and named best ophthalmology resident and received the Major David S. Berry Graduate Medical Education Top Resident Award. Dr. Reed is a board-certified ophthalmologist and is the current American Academy of Cosmetic Surgery Facial Cosmetic Surgery fellow at Texas Oculoplastics Consultants, TOC Eye & Face under the guidance of Tanuj Nakra MD.
Abstract
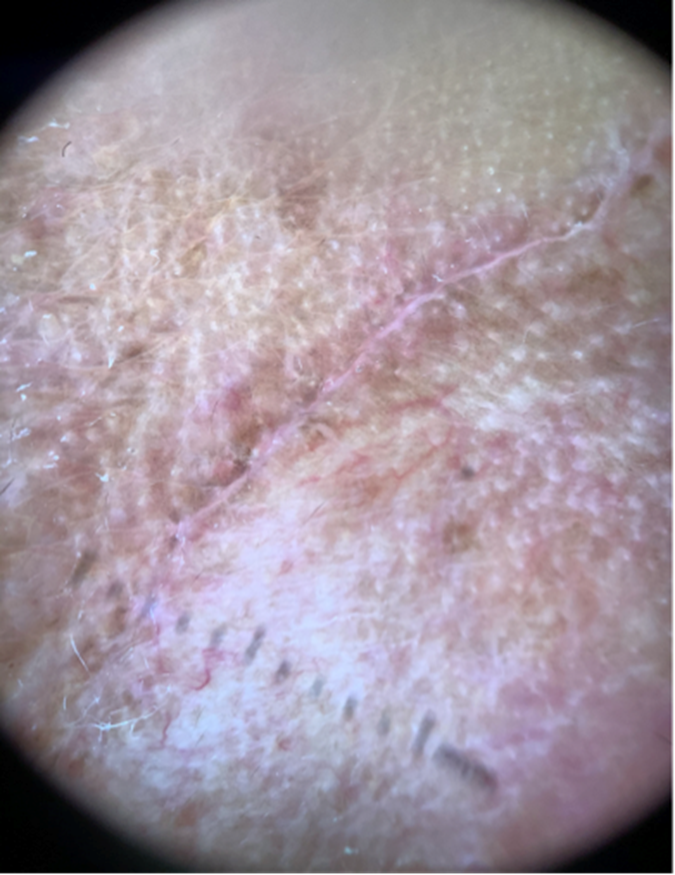
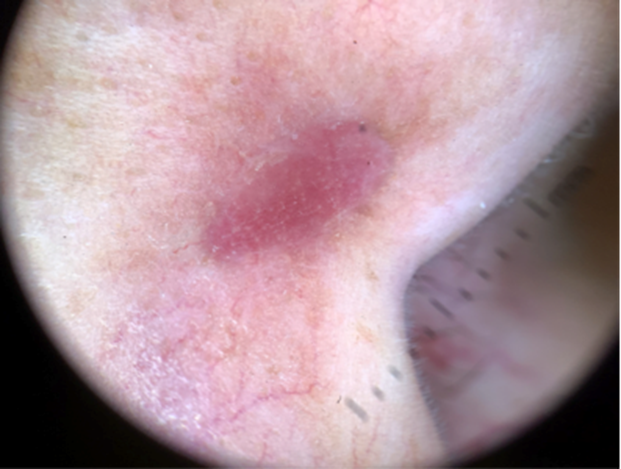
Introduction: Dermoscopy, or epiluminescence microscopy, allows the clinician to observe and analyze skin lesions without the obstruction of skin surface reflections.1-2 Dermoscopy has been noted to increase the sensitivity for skin cancer detection, decrease biopsy of benign lesions, and enable diagnosis of thinner malignancies. 3-10 The utility of dermoscopy in analyzing scar healing, vascularity and pigmentation has been demonstrated.12-16 In this study, we aimed to evaluate dermoscopy as an objective assessment tool for analysis of scar maturation vascularity, pigmentation, and depth to better inform treatment.
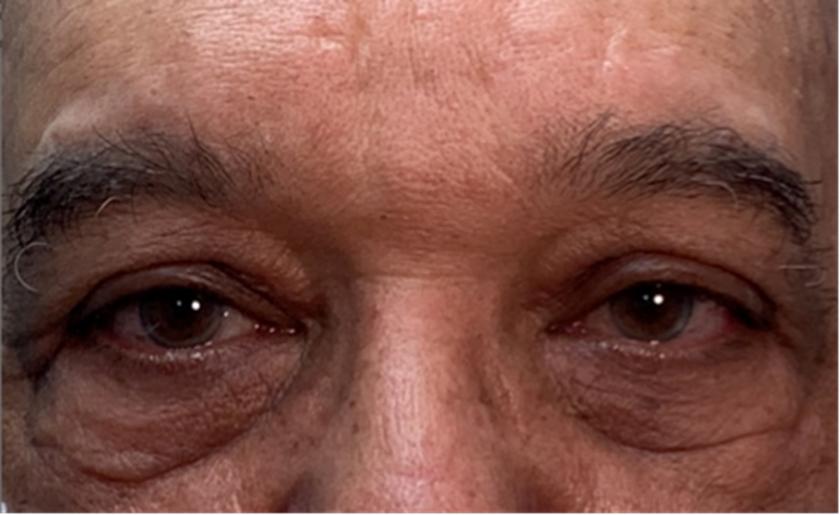
Methods: Sequential patients presenting to a facial cosmetic surgery practice with routine post-surgical facial scars were evaluated with and without the assistance of dermoscopy. Standardized photographs were taken with the dermoscope. Specific factors, including depth, vascularity, pigmentation, and content components (if applicable) were assessed by the surgeon initially without, and then with the assistance of a dermatoscope. Specific factors that either aided or altered the decision-making process were assessed. This study was exempted by the University of Texas Dell Medical School Institutional Review Board and adhered to the Declaration of Helsinki.
Results: A total of 50 scars were evaluated. Overall, surgeons found the dermatoscope to be superior to the naked eye in identifying depth, pigmentation, and vascularity of facial scars. Furthermore, vascularity and dermoscopic patterns were more apparent compared to slit-lamp exam. Specific factors found to be most useful for management decisions were depth and vascularity of the scar. The ability to obtain high-quality magnified photographs directly from the dermatoscope and upload the images into the patient’s electronic medical record (EMR)
Conclusions: Dermoscopy is an affordable and portable device that may be easily implemented in clinical practice, and it offers additional insights beyond slit-lamp examination. Dermoscopy is a valuable tool that can aid the clinician in highlighting features of facial scars that may inform treatment implementation. Finally, the ability to upload high-quality magnified images directly into the patient’s EMR was noted to be beneficial in monitoring progress and informing treatement decisions. Interventions undertaken in this patient cohort in concert with dermoscopic surveillance included application of topical corticosteroids, silicone and hydroquinone, as well as microneedling with 5FU (include reference), intense pulsed light (IPL) treatment, and scar revision.
Bibliography:
- Russo T, et al. Dermoscopy of malignant skin tumors: what’s new?. Dermatology. 2017. 233(1):64-73.
- Weber P, Tschandl P, Sinz C, Kittler H. Dermatoscopy of neoplastic skin lesions: recent advances, updates, and revisions. Curr treat options oncol. 2018. 19(11):56.
- Wozniak-Rito A, Zalaudek I, Rudnicka L. Dermoscopy of basal cell carcinoma. Clin Exp Dermatol. 2018. 43(3):241-47.
- Lallas A, et al. Dermoscopy in the diagnosis and management of basal cell carcinoma. Future Oncol. 2015. 11(22):2975-84.
- Lallas A, et al. Accuracy of dermoscopic criteria for discriminating superficial from other types of basal cell carcinoma. J Am Acad Dermatol. 2014. 70(2):303-11.
- Zalaudek I, Argenziano G. Dermoscopy of actinic keratosis, intraepidermal carcinoma and squamous cell carcinoma. Curr Probl Dermatol. 2015;46:70-6.
- Non-invasive diagnostic techniques in the diagnosis of squamous cell carcinoma. J Dermatol Case Rep. 2015. 31;9(4):89-97.
- Cheng CY, Su HJ, Kuo TT. Dermoscopic features and differential diagnosis of sebaceous carcinoma. J Dermatol. 2020. 47(7):755-62.
- Satomura H, Ogata D, Arai E, Tsuchida T. Dermoscopic features of ocular and extraocular sebaceous carcinomas. J Dermatol. 2017. 44(11):1313-16.
- Bryden AM, Dawe RS, Fleming C. Dermatoscopic features of benign sebaceous proliferation. Clin Exp Dermatol. 2004. 29(6):676-7.
- Yoo M.G., Kim I.-H.: Keloids and hypertrophic scars characteristic vascular structures visualized by using dermoscopy. Ann Dermatol 2014; 26: pp. 603-609.
- Deng H, Li-Tsang CWP, Li J. Measuring vascularity of hypertrophic scars by dermoscopy: construct validity and predictive ability of scar thickness change. Skin Res Technol. 2020. 26(3):369-75.
- Wei Y., Li-Tsang C.W.P., Luk D.C.K., Tan T., Zhang W., Chiu T.W.: A validation study of scar vascularity and pigmentation assessment using dermoscopy. Burns 2015; 41: pp. 1717-1723.
- Deng H, Li-Tsang CWP. Measurement of vascularity in the scar: a systematic review. Burns. 2019. 45(6):1253-65.
- Moscarella E, Argenziano G, Lallas A, Longo C, Jalbout SA, Zalaudek I. Pigmentation in a scar: use of dermoscopy in the management decision. J Am Acad Dermatol. 2013. 69(3):e115-6.
Take Home Message
Dermoscopy is a valuable tool that can aid the clinician in highlighting features of facial scars that may inform treatment implementation.